
Electron micrograph of a mast cell with many homogeneous granules. from "The in vitro differentiation of mast cells" by Ginsburg and Lagunoff, Journal of Cell Biology, 1967.
About the Lab
In the Mathias Lab, we primarily study mast cells and the interactions of mast cells with other immune cells during allergic responses. Although, our major interest is the investigation of the mechanisms underlying mast cell responses to oral and airway antigens, we follow the science wherever it leads us…including elucidating new roles for mast cells and other immune cells during disease pathogenesis.
Below is a brief introduction to mast cells and some of our research interests:
What’s in a cell? Pinging the mast cell.
Have you ever wondered why you had that sudden knee-jerk reaction causing you to sneeze when someone dumped a scoop of black pepper on their pasta? Or why you got a welt after that wasp bite you just had? How about that runny nose you always get soon after the dandelions rear their heads in the Spring? Or why some people have such a dire reaction to peanut? Well, one common cause of all of these disparate yet similar events is the immune cell we call the mast cell.
Mast cells were discovered by the German scientist Paul Ehrlich in 1877. He observed that these cells contained many granules, which he believed were responsible for nourishing the surrounding tissue. He therefore called them mastzellen for “fattening”. Mast cells have come a long way since that early discovery. We now know that mast cells are a type of white blood cell that not only protect us from infectious diseases, but are also responsible for causing many of the symptoms we associate with allergic diseases. The histamine released by these cells also plays a major role in facilitating physiological responses to inhaled or ingested foreign particles by stimulating smooth muscle receptors and causing spasms that result in ejection of the foreign substance. So, the next time you sneeze or cough when you feel that tickle in your nose, definitely think mast cells. Of course, these cells are only one part of the entire equation, as the reflex reaction you experienced is a manifestation of the perfect scenetta choreographed by components of the immune and nervous systems.
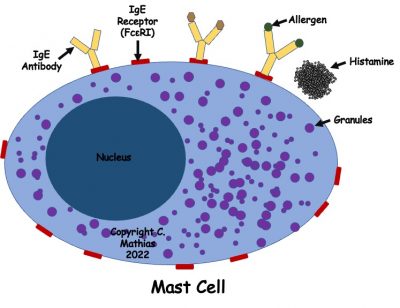
So, what actually do mast cells do? Evolutionarily, mast cells seem to be pretty conserved. Their fattened granules contain many substances such as histamine and protein-degrading chemicals called tryptases that can increase blood flow and inflammation and destroy pathogens. In humans, mast cells are well known for curbing diseases caused by parasites and helminth worms such as roundworms and hookworms in coordination with antibodies produced by the immune system, called IgE antibodies. In the last century, the role of mast cells in propagating allergic diseases has also become very clear.
So what exactly do we do in our laboratory? In our lab, we are very interested in determining the various factors that can influence mast cell behavior during allergic diseases. Our lab has a special interest in studying food allergy and we examine factors that can promote or suppress mast cell functions during food allergy responses. Some factors we have been examining include diet, chemical modifications affecting gene expression, the role of chemical messengers produced by immune cells.
Diet – Diet has a major impact on our lifestyle. Recent evidence also shows that diet can have an enormous impact on the immune system. In the case of allergic diseases in particular, it appears that people in Western countries seem to experience many more episodes of allergic disease compared to those in the East. We wondered whether diet may have any role to play in this and if dietary factors could influence mast cell responses during food allergy. One particular factor we honed in on was the active ingredient of the curry spice turmeric. This compound, curcumin by name, is known to have anti-inflammatory and anti-oxidant functions, and we hypothesized that frequent consumption of curcumin through diet may affect mast cell growth and its activation and functions in the gut. We found that feeding mice with curcumin during food allergy responses suppressed mast cell growth, reduced its activation via IgE antibodies, and decreased the amount of chemical messengers called cytokines produced by these cells. The net effect was a decrease in food allergy symptoms. This paper is published here (https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0132467), and we are continuing to look at the effects of diet on food allergy under various circumstances.
Epigenetic regulation: In recent years, there has been a major breakthrough in our understanding of how genes control our behavior and other physiological responses. The importance of genes in the expression of proteins and many of the phenotypical behaviors observed in various diseases is well-understood. For example, certain genes can be pinpointed as culprits in inherited diseases such as Huntington’s or muscular dystrophy. But then there are other diseases such as asthma or some autoimmune diseases that present with many variations in the human population, the causes of which cannot be explained by a single genetic defect alone. The presence of multiple alleles or copies of genes within the human population, what scientists refer to as genetic polymorphism, may be one explanation for this variegated presentation. Recent discoveries however show that simple chemical modifications to genes, often resulting from certain types of environmental stresses or exposures, can cause them to be expressed or repressed in individuals of diverse genetic backgrounds. These modifications may be as simple as addition of what we call methylated groups to DNA sequences or changes in proteins called histones that hug DNA tightly giving rise to its supercoiled conformation. This suggests that individuals do not have to be born with a certain genetic defect to manifest a variation of a disease, but environmental exposures during their lifetimes could chemically modify the DNA in disease-associated genes causing them to behave one way or another. In some cases, these DNA patterns can be imprinted and transmitted to progeny. In our studies, we have found that inhibiting histone deacetylation during food allergy, by using a histone deacetylase inhibitor called trichostatin A, can suppress mast cell activation and functions during food allergy, resulting in decreased food allergy symptoms (https://www.frontiersin.org/articles/10.3389/fimmu.2018.02414/full). We are continuing to explore other modes of epigenetic regulation of mast cells during allergic responses.
Cytokines: Chemical messengers called cytokines play vital roles during immune responses. These small molecules released by cells allows them to communicate with other cells by binding receptors on those cells that transmit signals into the cell’s interior via enzymatic activity. These signals cause the cells to behave in a specific fashion or express or repress specific genes. Cytokines can also act on the cells producing it and can regulate its own activity via positive or negative feedback activity, i.e., promoting a certain activity by the cell or suppressing it. A number of cytokines are known to affect mast cell growth and regulate its functions. We recently found that the cytokine, called interleukin-10 or IL-10, known to be a major player in the immune system, can regulate mast cell growth and function by promoting its activity during allergic responses. IL-10 is actually notorious in the immune response for regulating immune activity and suppressing immune responses after they have accomplished their protective functions. For example, an infection in the GI tract might call for an overwhelming immune response that targets the offending bacteria and eliminates the infection. Once the infection is controlled, the immune response needs to subside so as not to inadvertently harm the person’s own cells and organs, and healing of tissues needs to occur. IL-10 is a cytokine produced by immune cells that suppresses the inflammation and allows healing to occur. We have found, on the other hand, that IL-10 is a potent stimulator of mast cells (https://www.jimmunol.org/content/196/12/4865.long). Not only does it promote mast cell growth during food allergy, but it can also stimulate its proliferation and survival during normal physiological conditions. Moreover, IL-10 potently enhances the production of other pro-allergic cytokines released by activated mast cells, further potentiating their effects and enhancing the overall symptoms of food allergy. We are now examining the effects of IL-10 on mast cells in much more detail and assessing the responsiveness of various mast cell subsets under varying conditions to IL-10 stimulation.


